SUMMARY: Malassezia typically causes skin infections but can occasionally cause systemic disease, particularly in patients with indwelling devices such as central venous catheters. Dr Pedrosa and colleagues have published a literature review and three unrelated cases of systemic Malassezia at a hospital in Portugal.
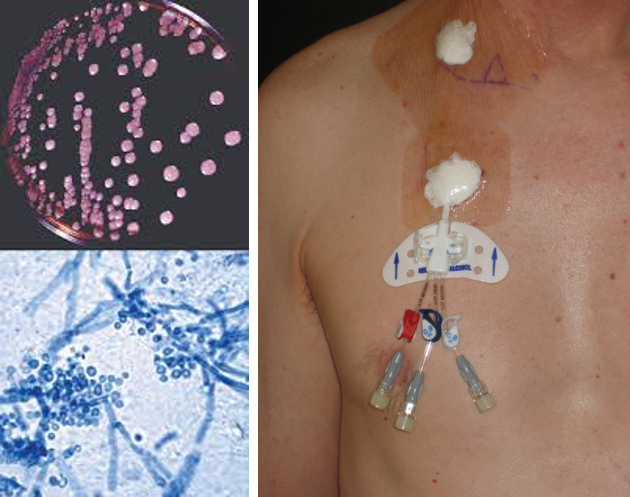
Malassezia spp. (formerly Pityrosporum) are commensal yeasts that typically cause skin infections, but preterm infants and immunocompromised patients are at risk of life-threatening systemic involvement, often via indwelling medical devices. While the prevalence of systemic infections is low, mortality is high — partly because diagnosis (and therefore treatment) is often delayed. Clinical course is often indolent, with non-specific symptoms such as fever of unknown origin. In addition, laboratory culture requires non-standard media containing lipids, and susceptibility testing is not routinely available.
Dr Ana Filipa Pedrosa and colleagues in Porto (Portugal) have published a series of 3 unrelated cases of Malassezia bloodstream infection with an accompanying literature review. All 3 patients had a central venous catheter 2yo female in paediatric ward for fever of unknown origin. Glucocorticoid therapy and autoimmune disease (reduced IL-12). On broad-spectrum antibiotics. Received fluconazole and liposomal AmB, survived but contracted pityriasis versicolor 3 years later. 68yo female in ICU for systemic inflammatory response syndrome. HIV+ on HAART, with chemotherapy for oral carcinoma. On fluconazole prophylaxis. Received liposomal AmB but died after 15 days. 60yo male in ICU for acute respiratory distress syndrome. HIV+ on HAART, with chemotherapy for Hodgkin disease. On fluconazole prophylaxis. Received liposomal AmB but died after 3 days.
What can I do?
- NICU clinicians: be aware that infections are more likely when infants are receiving lipid infusions (on TPN)
- Blood cultures are the gold standard for diagnosis, and should be supplemented with lipids (e.g. palmitic acid, sterile olive oil) and incubated for up to 2 weeks. Identification to species level requires molecular tests or MALDI-ToF, and is not generally required for clinical management
- If a central venous catheter is involved, remove it promptly
- For patients who develop this infection while under fluconazole prophylaxis, use amphotericin B as first-line treatment but be aware that susceptibility profiles are not well characterised for this group of yeasts